The Most Advanced Corneal Solutions
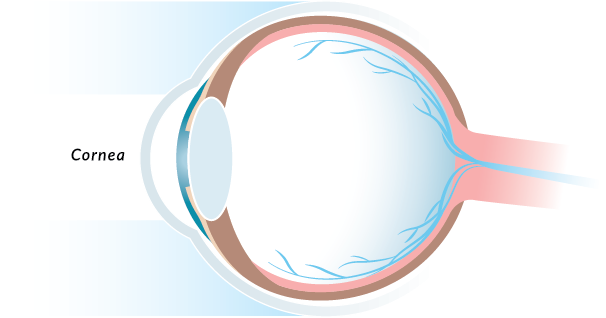
If you begin to experience issues with your vision, such as dry eye, eye pain, or blurred vision, it may be a sign of a corneal issue. But what exactly is the cornea? The cornea is your eye’s outermost layer and provides most of the focusing power of the eyes. When there is a problem with your cornea, it can significantly affect your vision and cause long-term damage. At Wilmington Eye, our highly specialized corneal team offer the broadest and most advanced corneal solutions, providing exceptional corneal care to patients across southeastern North Carolina.
Detecting & Treating Dry Eye Disease
One of the most commonly treated corneal issues is Dry Eye Disease. If you have prolonged symptoms of dry eyes, red or irritated eyes, stinging and burning or even tired or painful eyes, you may be suffering from Dry Eye Disease. Dry Eye Disease occurs when your tears are no longer able to provide adequate lubrication for your eyes. If you suspect that you may be suffering from Dry Eye Disease, it’s important to see your eye doctor. The most common treatment for Dry Eye Disease is over-the-counter artificial tears. However, patients that experience more severe or persistent symptoms may require additional procedures or surgery to repair or manage the underlying cause of dry eye. Our cornea specialist will meet with you to determine the best possible treatment plan for you.
OTC Products for Dry Eye
Wilmington Eye offers over-the-counter products for Dry Eye so that you can leave your appointment and immediately begin your treatment plan, skipping the long lines at your pharmacy or local drug store.
- Artificial Tears
- Serum Tears
- Punctual Plugs
Treatments for Dry Eye
When over-the-counter products fail to provide relief from Dry Eye, Wilmington Eye offers several in-office treatments that can alleviate the symptoms of Dry Eye and directly treat the ocular disease.
- Lipiflow
- IPL (Intense pulsed light therapy)
- Maskin Probe
Other Corneal Problems & Diseases
While Dry Eye is a common corneal-related problem that we treat, our board-certified ophthalmic surgeons specialize in other conditions of the cornea. If you begin to experience any changes in your vision, have sudden or severe pain, or have been diagnosed with a corneal disease, it may be time to see a corneal specialist. Some common corneal diseases include:
- Conjunctivitis (Pink Eye)
- Corneal Infections
- Dry Eye
- Fuchs’ Dystrophy
- Corneal Dystrophies
- Herpes Zoster (Shingles)
- Keratoconus
- Epithelial Basement Membrane Dystrophy
- Ocular Herpes
- Pterygium
Advanced Corneal Procedures
If you have been diagnosed with a corneal disease, it’s important to seek treatment immediately. Our experienced cornea doctor, Dr. Clark Springs, has more than 15 years of experience treating corneal issues and diseases. We will evaluate your vision to determine the root cause of your vision problems and develop a custom treatment plan that utilizes the latest in prescription drugs and medical technology to deliver lasting results and improve your vision. In addition to superior care, our corneal team provides some of the most advanced and proven treatments for corneal disorders, including:
- Full & partial corneal transplants
- Ultra-thin Endothelial Keratoplasty (DSEK)
- Superficial Keratectomy
- Lipiflow
We are proud to have one of the most talented corneal specialists in the region. Our highly specialized corneal team offer complete care, from diagnosis and treatment to post-operative care. If you are experiencing an issue with your vision, schedule an appointment with our doctors today.